
In 2018, the Indian Government launched its flagship Ayushman Bharat scheme, making a major step towards India’s commitment to achieving UHC. This comprised of two critical components: Health & Wellness Centres – also known as Ayushman Arogya Mandirs – to strengthen public primary healthcare services. Alongside this, the Pradhan Mantri Jan Arogya Yojana was introduced to provide financial protection for low-income households.

HWCs or AAMs are designed to deliver comprehensive PHC services that go beyond the earlier focus on maternal and child health, infectious diseases, etc. They now include screening and management of chronic illnesses, a new cadre of public primary health care officers, digital reporting systems closer to communities. They are also envisioned as a referral link to higher-level care.

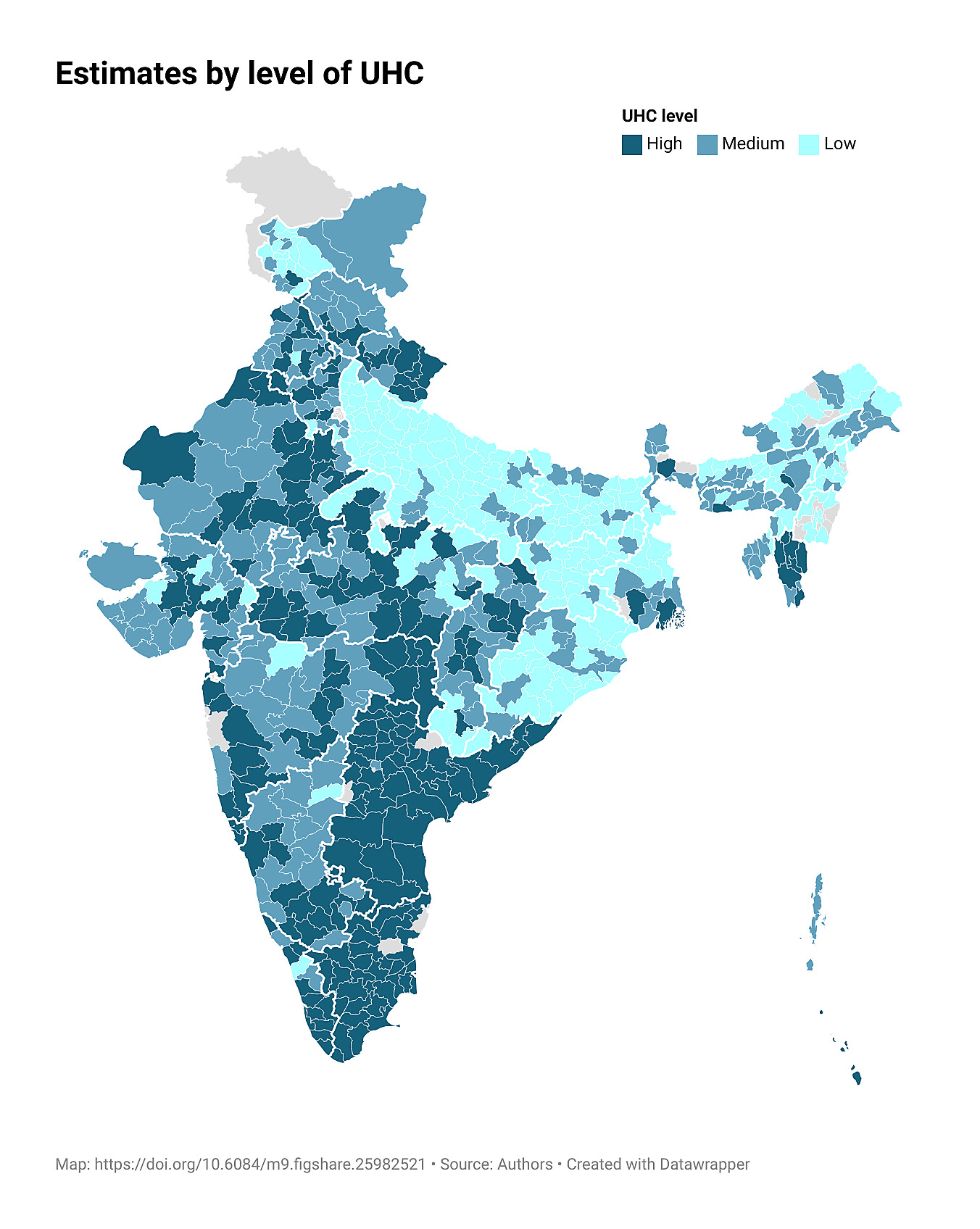
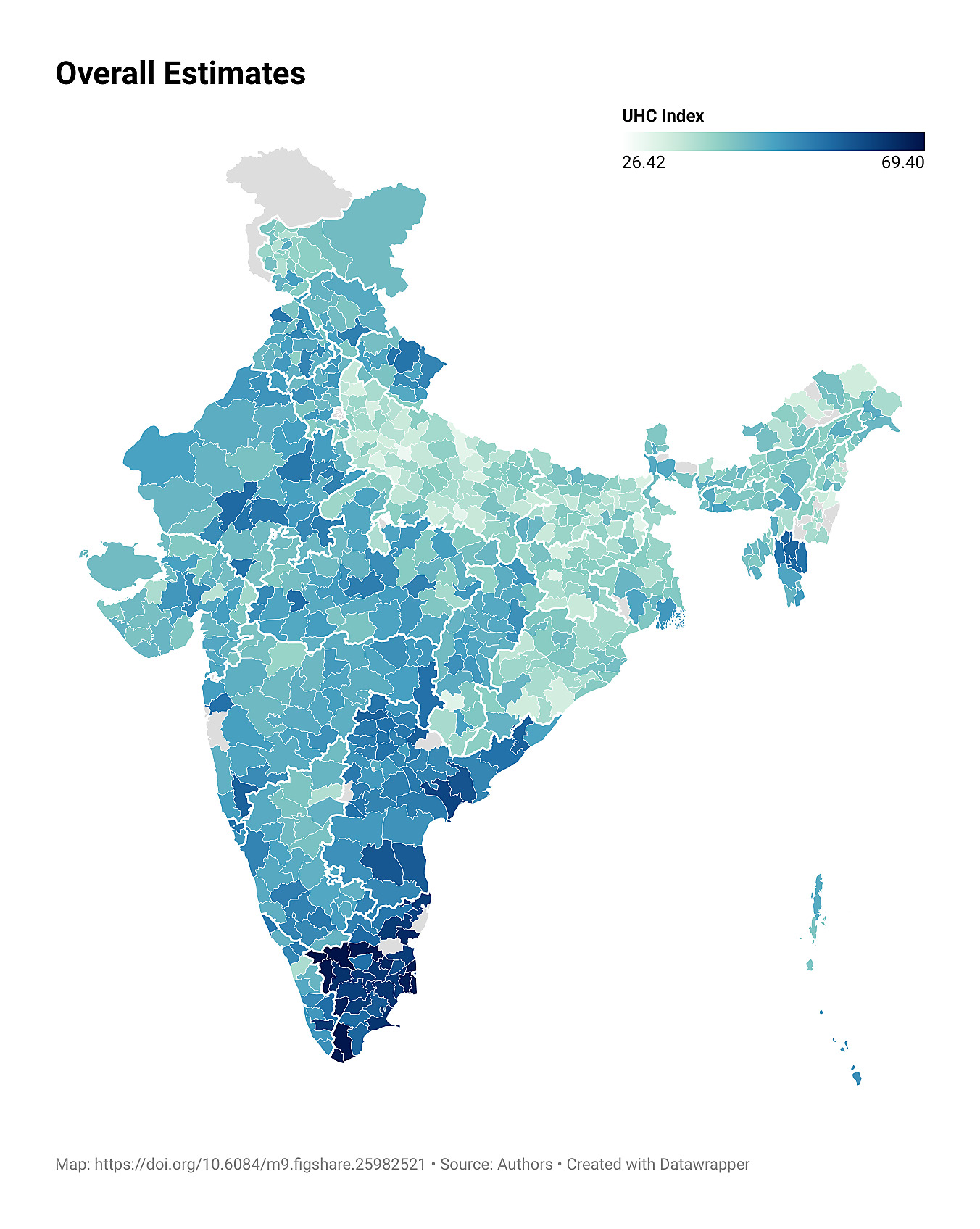
In India’s federal health system, states have taken diverse routes towards UHC. State-level priorities have shaped diverse reforms, models and pathways, further influenced by contexts and resources. Research led by investigators in this consortium using an adapted WHO-World Bank UHC Index has found wide variation in UHC levels across the country. (Mukherji et al. 2024) Drawing on earlier in-depth qualitative health system research, we found how context – including epidemiological stages, health system structures, socio-political history – have shaped India’s many pathways to UHC. For instance, in states with a strong history of community engagement tend to emphasise decentralised, bottom-up approaches while others have focused on expanding health insurance coverage.
Additionally, the relationship between PHC and UHC is often conceptualized as a structured pathway, where PHC serves as the organizing strategy that translates systemic goals into tangible health outcomes. Crucially, the operationalization of this pathway depends on robust, context-sensitive measurement of PHC. Without systematic monitoring of both inputs and service delivery outputs at district or facility levels, policymakers lack the evidence required to track progress and ensure that UHC commitments are translated into equitable, high-quality, and people-centred care at the community level.
The PHC4UHC is an Indian research consortium examining the different pathways through which PHC approaches, as designed, and implemented in India, contribute to progress in UHC. It is funded by the WHO Alliance for Health Policy and Systems Research for the period 2023–2025.
How PHC processes improve UHC outcomes:
Evidence synthesis of what works, for whom, where.
How PHC and UHC are correlated in India:
Secondary analysis of UHC indices and PHC inputs
How do PHC interventions improve UHC outcomes?
Case studies of 3 interventions at the district-level in two states

We conducted a realist review of evidence on UHC outcomes – population, service, and financial risk protection – to identify the contribution and role of PHC approaches, unpacking the processes and contexts through which PHC mechanisms have yielded impact in 20 countries with the highest absolute increases in UHC Service Coverage Index scores (2000-21).

We compiled and analysed relevant secondary data across multiple national sources, to examine the status of primary healthcare service coverage by developing a district-level PHC inputs index, with a focus on Karnataka and Jharkhand. By developing a PHC Inputs Index and linking it to a UHC Index, we explored how PHC investments translate into progress toward UHC using a distinct set of measurable indicators for each.